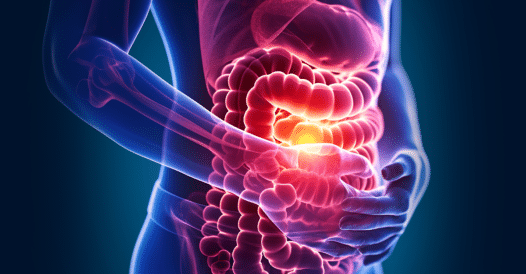
Challenges abound for patients and clinicians alike when it comes to managing gastrointestinal diseases, making it imperative that all stakeholders on the care team—including the patient—continue to hone their knowledge, confidence, and best practice strategies to improve outcomes. CME Outfitters’ Gastroenterology Education Hub provides clinicians with the education and resources necessary to optimize their approach to clinical care for patients with inflammatory bowel disease, irritable bowel syndrome, chronic idiopathic constipation, and diabetic gastroparesis.
- Activities▼
- Education Hubs▼
-
- Alzheimer’s Disease
- Cardiology
- COVID-19
- Dermatology
- Gastroenterology
- Health Access & Social Responsibility
- Hematology
- Immunodeficiency Disorders
- Infectious Disease
- Liver Disease
- Metabolic Diseases Education
- Migraine
- Multiple Sclerosis
- Neuropsychiatric
- Oncology
- Ophthalmology
- Pain Management
- Pediatrics
- Pharmacist Central
- Psoriatic Arthritis
- Rare Diseases
- Respiratory
- Rheumatology
- Sleep Disorders
- Transplant
- Virtual Education
-
- Services▼
- News▼
- ▼