As Bleeding Disorder Awareness Month comes to an end, CME Outfitters would like to shine a light on von Willebrand disease (VWD), a rare bleeding disorder which affects approximately 1%-2% of the United States.
Von Willebrand disease is the most common inherited bleeding disorder and is caused by a deficiency in, or dysfunction of, von Willebrand factor (VWF). Symptoms of VWD range from mucocutaneous bleeding to gastrointestinal bleeding to joint arthropathy. People who have uteruses carry an additional burden and may face chronic menstrual bleeding.
We sat down with Brandee Cookston and Nikki Angeles from VWD Sisterhood, a patient advocacy group that provides support for people living with VWD.
Hey, Brandee & Nikki, please introduce yourselves and tell us your VWD story.
 Brandee: My name is Brandee, I live in a small town on the Gulf Coast of Alabama, and I live with von Willebrand Disease (VWD). I was your average child growing up. That is, until I was 12 years old and started my first menstrual cycle. Who knew that after that day, my life would forever change? (I sure didn’t!) After bleeding heavily for over 30 days, I went to my pediatrician to see if we could figure out what was happening. A few days later, her suspicions were correct. It was VWD, and I would need to see a hematologist. It took several years and numerous birth control pills and factor products to get my cycles under control.
Brandee: My name is Brandee, I live in a small town on the Gulf Coast of Alabama, and I live with von Willebrand Disease (VWD). I was your average child growing up. That is, until I was 12 years old and started my first menstrual cycle. Who knew that after that day, my life would forever change? (I sure didn’t!) After bleeding heavily for over 30 days, I went to my pediatrician to see if we could figure out what was happening. A few days later, her suspicions were correct. It was VWD, and I would need to see a hematologist. It took several years and numerous birth control pills and factor products to get my cycles under control.

Nikki: My name is Nikki and I have been diagnosed with VWD type 1 severe. I was diagnosed at the age of 16 after a very serious hemorrhage in the middle of the street. I began my journey of controlling my bleeds with several forms of oral contraceptives and trials of IV infusions.
What are some of the challenges you’ve faced as someone living with VWD?
Brandee: For years I suffered, begging my gynecologist for a hysterectomy. I was receiving several units of blood a month to keep up with my blood loss. I had no quality of life. I desperately wanted my life back. I realized that my gynecologist was never going agree to give me a hysterectomy, and it was time to part ways. Within three months of seeing a new gynecologist, I had my hysterectomy. Finally, after years of suffering, I began to take my life back.
Nikki: During the early days of my diagnosis, I had to decide to either have a hysterectomy or to become pregnant. I had to make that decision quickly due to my severe bleeding and the intense pain I was experiencing. I eventually decided to have a baby after becoming a part of the bleeding community and finding a better health care team. I continue to experience recurrent left elbow joint bleeds and heavy menstrual bleeds.
How does VWD affect your daily life?

Brandee is able to do in-home treatments like infusions.
Brandee: Since having my hysterectomy, I don’t have as many bleeding issues. That’s not to say that I don’t suffer from bruising and occasional joint bleeds, because I do. I try to be more cautious in my day-to-day activities. Is the risk worth the reward? In most cases, it’s not. If I want to do an active activity, I must infuse beforehand. Now that I’m in my thirties, the activity has to be something pretty amazing for me to pretreat. I also receive prophylactic treatment every week, which has been a godsend to help with my bruising and pain in my joints.
Nikki: Since I live with a port, I am very careful and mindful of my safety. Due to the recurrent joint bleeds in my left elbow, it does not fully extend and is very painful daily. Since I experience heavy menstrual cycles, I am very cautious about where I travel, and how I travel. I live with anxiety, as I fear embarrassment.
Why is community support important for VWD patients?
Brandee: Four months after my surgery, I attended a conference specifically for VWD patients. That conference changed my life, not just from a medical standpoint, but because of the lifelong friendships I made with people from all over the United States. I feel that it is so important to immerse yourself within this community. These are people who will truly understand everything that you go through. They will be your biggest supporters and advocate right alongside you.
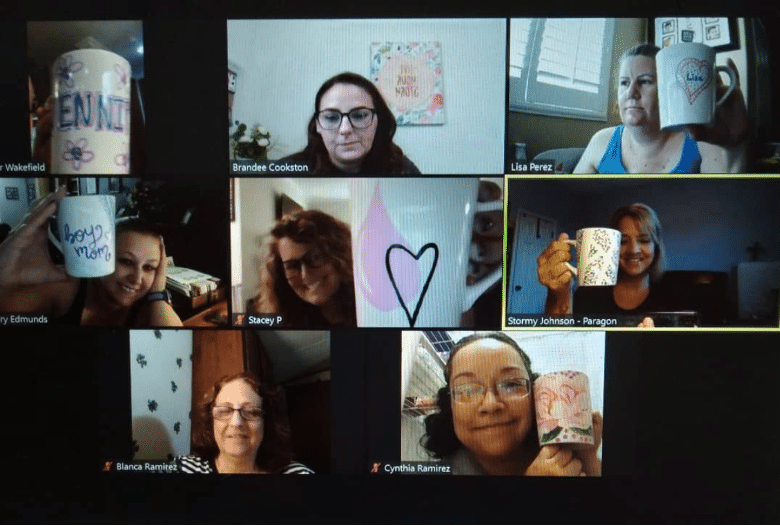
The nation-wide VWD Sisterhood regularly meets on Zoom.
How did the VWD Sisterhood come to be?
Brandee: VWD Sisterhood started as a support group at the beginning of the pandemic. We have grown into something within our community that I could have never fathomed. Our main objectives and goals are to provide women with the education and support they may need, whether being a patient advocate for them or just a sister to lend an ear. We want them to know they aren’t alone in this battle. There is an army of women behind them, ready to fight.
Nikki: We stand behind patients who live with VWD, especially the people who suffer with their menstrual cycles. There is a myth that only men can live with bleeding disorders and VWD Sisterhood is fighting back. We have a strong foundation and will continue to grow. The DOT BOX we send out monthly is to show our sisters – during even the hardest times – WE are here for them.
“Our main objectives and goals are to provide women with the education and support they may need, whether being a patient advocate for them or just a sister to lend an ear. We want them to know they aren’t alone in this battle.”
So, what is the DOT BOX?
Nikki: The monthly DOT BOX is to show our sisters that during the hardest times, WE are here for them. We came up with this idea because one of the biggest challenges women face is menstruation. When we speak to our providers, a lot of the times they do not provide comfort or truly understand our troubles. We want to provide comfort, be the shoulder they need, and show them WE HEAR THEM.

VWD Sisterhood sends a “DOT BOX” to one of its members each month as a way of showing support during menstrual cycles.
What are some of the challenges faced by patients with VWD, and how can clinicians better address these challenges?
Brandee: As VWD patients, we face a lot of different challenges. Even more so for women. Clinicians need to realize that gender shouldn’t dictate how they treat their patients. More often than not, females will receive less optimal care than male patients. Clinicians dismiss our symptoms. Why? Why are men’s symptoms more believable? Re-educating our clinicians should be a top priority. They need to learn to look past the gender, listen to the patient, and treat accordingly.
Nikki: VWD patients face the challenge of not being heard and feeling left behind. Clinicians need to stop and listen to VWD patients. They also need to understand that every VWD patient is different. It is all about taking the time to listen and map out a plan to keep the patient safe and happy. Clinicians can make a change by putting VWD patients at the same level of care as hemophilia patients. Often, VWD is evaluated by its type rather than the patient’s testimony. They should ask what we want, instead of telling us what we want.
“It took me years to receive prophylactic treatment. It has made a huge difference in my life; I only wish my doctor would have allowed me to do it sooner.”
How can providers bridge gaps in care?
Brandee: Providers should educate themselves on the new guidelines for VWD management, listen to their patients, and provide them with prophylactic treatment options. It took me years to receive prophylactic treatment. It has made a huge difference in my life; I only wish my doctor would have allowed me to do it sooner.
Nikki: What is not discussed often is that VWD patients can live with a prophylactic treatment plan. I personally believe that this would be a huge game changer within the community. Providers should focus more on treatment plan options outside of contraceptives. Providers should look more into VWD research and therapies. Women should have a voice and not be given ultimatums.
Thank you so much for providing these valuable insights. The patient perspective is so important! Any closing thoughts?
Nikki: What is not discussed often is that VWD patients can live with a prophylactic treatment plan. I personally believe that this would be a huge game changer within the community. Providers should focus more on treatment plan options outside of contraceptives. Providers should look more into VWD research and therapies. Women should have a voice and not be given ultimatums.
Brandee: If you would have said at the beginning of my VWD journey that this is where I would end up, I wouldn’t have believed it. I am so thankful that sharing my journey will help others.
If you are a woman living with VWD in the US, you can join the VWD Sisterhood community on Facebook and Instagram.
Clinicians, for additional education on bridging gaps in diagnosing, treating, and managing VWD, view our OnDemand CME/CE webcast.
*Note: This interview has been edited for length and clarity.

About the Author
Gillian Booth
Marketing Associate, CME Outfitters