Continuing towards a goal of safe opioid prescribing in those with acute and chronic pain, part 2 of our 3-part opioid education series will speak to best practices for evaluating and managing a patient in pain. In the last section of this opioid education series we recapped expert insights from our Opioid Healthcare Provider/Advocacy Working Group two-day advisory board meeting. These insights and perspectives described the roles of various stakeholders in the opioid landscape, current attitudes towards patients with chronic pain, the CDC guideline for prescribing opioids for chronic pain, and an in-depth overview of pain, and the different pain mechanisms we experience.
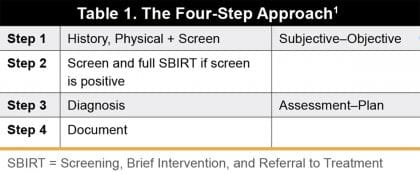 In order to provide effective and safe pain management, healthcare providers should perform a comprehensive assessment of their patient that includes a history and physical examination with screening for substance use to determine an appropriate treatment plan that safely meets the patient’s needs.1 A comprehensive assessment can be performed efficiently with standardized processes; however, multiple visits may be needed to complete the entire assessment. One possible method to consider is a four-step approach, which follows the SOAP (Subjective–Objective–Assessment–Plan) format (Table 1).
In order to provide effective and safe pain management, healthcare providers should perform a comprehensive assessment of their patient that includes a history and physical examination with screening for substance use to determine an appropriate treatment plan that safely meets the patient’s needs.1 A comprehensive assessment can be performed efficiently with standardized processes; however, multiple visits may be needed to complete the entire assessment. One possible method to consider is a four-step approach, which follows the SOAP (Subjective–Objective–Assessment–Plan) format (Table 1).
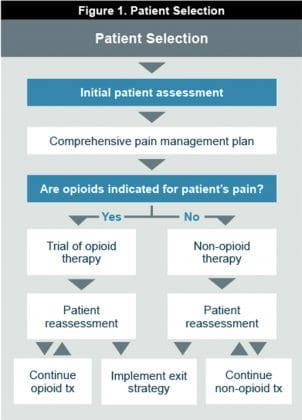 Providers should assess the patient’s pain including location, intensity, quality, etc; the effects of the pain on function and quality of life; comorbidities (eg, depression, anxiety); psychosocial history, including family history of substance abuse and psychiatric disorders, history of trauma/sexual abuse; mental health and functional status; medication and substance use history; past and current substance use disorders; and past pain management and coping strategies as well as maladaptive pain-related thought patterns.1 The patient history should include psycho-social stressors, family history, and pre-adolescent history. This comprehensive history and physical, and risk assessment at the initial evaluation are necessary to determine the appropriate pain management strategy (Figure 1).
Providers should assess the patient’s pain including location, intensity, quality, etc; the effects of the pain on function and quality of life; comorbidities (eg, depression, anxiety); psychosocial history, including family history of substance abuse and psychiatric disorders, history of trauma/sexual abuse; mental health and functional status; medication and substance use history; past and current substance use disorders; and past pain management and coping strategies as well as maladaptive pain-related thought patterns.1 The patient history should include psycho-social stressors, family history, and pre-adolescent history. This comprehensive history and physical, and risk assessment at the initial evaluation are necessary to determine the appropriate pain management strategy (Figure 1).
The risk of abuse should be evaluated using risk stratification and assessment tools. The presence of risk factors (eg, personal or family history of OUD, psychiatric disorder) may influence the choice of medication, follow-up, monitoring, and tapering protocols after surgical procedures. Urine drug testing (UDT) is an important component of risk management and should be completed in initial screening and annually during follow-up.2 UDT is an effective and cost-efficient method that facilitates objective assessment of treatment compliance. Although UDT is generally reliable, false positives can occur and confirmatory testing may be necessary.3
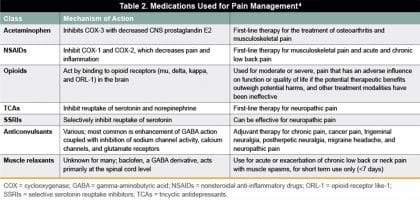 Table 2 shows several common nonopioid and opioid medications that can be considered for the management of acute and chronic pain.4 Medication selection is based on the severity of pain and injury.5,7
Table 2 shows several common nonopioid and opioid medications that can be considered for the management of acute and chronic pain.4 Medication selection is based on the severity of pain and injury.5,7
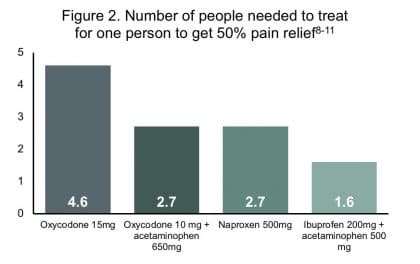
The most commonly used nonopioid medications are NSAIDs and acetaminophen. Several Cochrane reviews have been examined to compare agents in the treatment of post-operative pain. The Cochrane Collaboration applied number needed to treat (NNT) as the statistical measure for comparing pain relief effectiveness using the standard that 50% pain relief of pain is considered effective allowing for increased function and quality of life. Figure 2 compares NNT for opioids versus nonopioid formulations. A lower NNT equates to better pain relief.8-11
 A benefit-to-harm evaluation is necessary to assess the risk of pain versus the risk of opioid treatment for pain management. Pain is associated with decreased quality of life, reduced physical functioning, increased disability, and increased social costs (eg, work absenteeism, increased utilization of medical resources.6 Comorbidities associated with chronic pain include depression, sleep disturbances, and impaired memory, cognition, and attention. Pain is one of the most common reasons for outpatient visits in the United States.
A benefit-to-harm evaluation is necessary to assess the risk of pain versus the risk of opioid treatment for pain management. Pain is associated with decreased quality of life, reduced physical functioning, increased disability, and increased social costs (eg, work absenteeism, increased utilization of medical resources.6 Comorbidities associated with chronic pain include depression, sleep disturbances, and impaired memory, cognition, and attention. Pain is one of the most common reasons for outpatient visits in the United States.
The benefits of opioid treatment in the management of severe pain are analgesia (pain control) and improved function.5 Providers should be wary of overprescribing medication and consider the risks of treatment as part the benefit-to-harm evaluation. The potential risks of opioid treatment are considerable and include overdose; life-threatening respiratory depression; abuse, misuse, and addiction by patient or household contacts; physical dependence and tolerance; interactions with other medications and substances; and risk of neonatal withdrawal syndrome.12,13
The need for a change in opioid prescribing has been increasingly recognized to address overprescribing and the risk of abuse. The frequent prescribing of opioids for the treatment of dental pain was highlighted in a study by Mutlu et al, which surveyed 384 randomly selected oral and maxillofacial surgeons and found that the average number of tablets prescribed was 20, with 22% of oral surgeons prescribing more than 20 tablets and 11% prescribing more than 30 for postoperative pain following oral surgery.14 Yet Lahey et al examined 105 patients of 8 oral surgeons to determine the number of opioids actually used by patients following third molar surgery and found that only 38.4% of all prescribed opioids were consumed during the study period.49 Nonopioid analgesics should be the primary agents for managing postoperative dental pain. In a study of published systematic reviews, Moore examined the benefits and harms of analgesic medications used for the management of acute dental pain.16 Their findings supported the use of NSAIDs and acetaminophen to provide effective acute pain management.
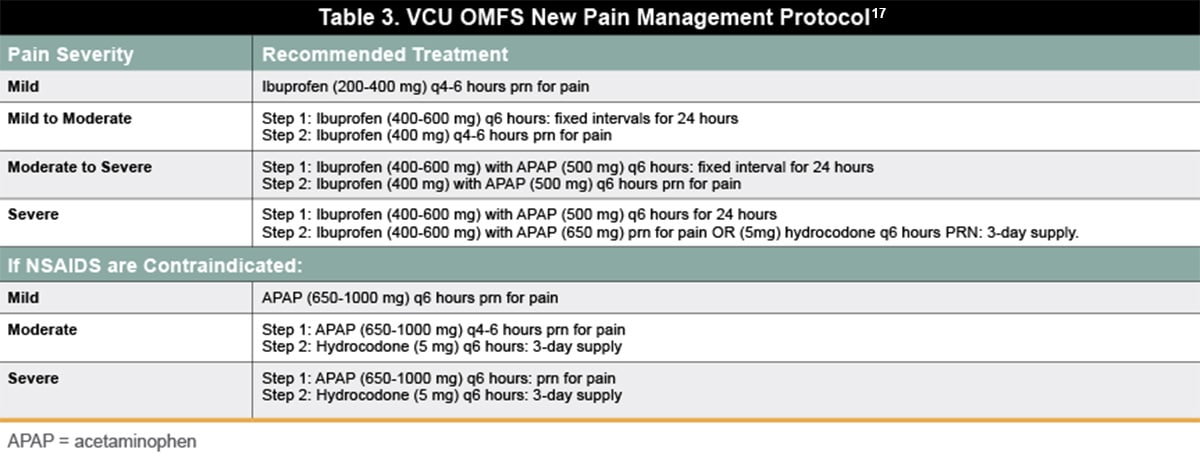 As an example of this shift pain management protocols, the Virginia Commonwealth University (VCU) Department of Oral and Maxillofacial Surgery has issued a set of pain management guidelines to assist in curbing the use of opioids for the treatment of dental pain.
As an example of this shift pain management protocols, the Virginia Commonwealth University (VCU) Department of Oral and Maxillofacial Surgery has issued a set of pain management guidelines to assist in curbing the use of opioids for the treatment of dental pain.
Recommendations for acute pain management following musculoskeletal injury include pain medication strategies, physical modalities, and system tools.18 Pain medication strategies may involve the use of multimodal analgesia, including NSAIDs, acetaminophen, gabapentinoids, and immediate-release opioids. Clinicians should prescribe the lowest effective immediate-release opioid dose for the shortest period possible and avoid prescribing extended-release opioids. Local or regional block anesthesia can be considered as part of a postoperative multimodal regimen. Physical modalities may include the use of appropriate immobilization, ice, and elevation; transcutaneous electrical stimulation; and cryotherapy. System tools that are available as part of acute pain management are state prescription drug monitoring programs (PDMPs), which should be queried before prescribing opioids; clinical decision support for opioid prescribing in the electronic medical record; and opioid education efforts for prescribers and patients. Assessments for pain and sedation should be performed regularly for inpatients and outpatients with short validated tools.
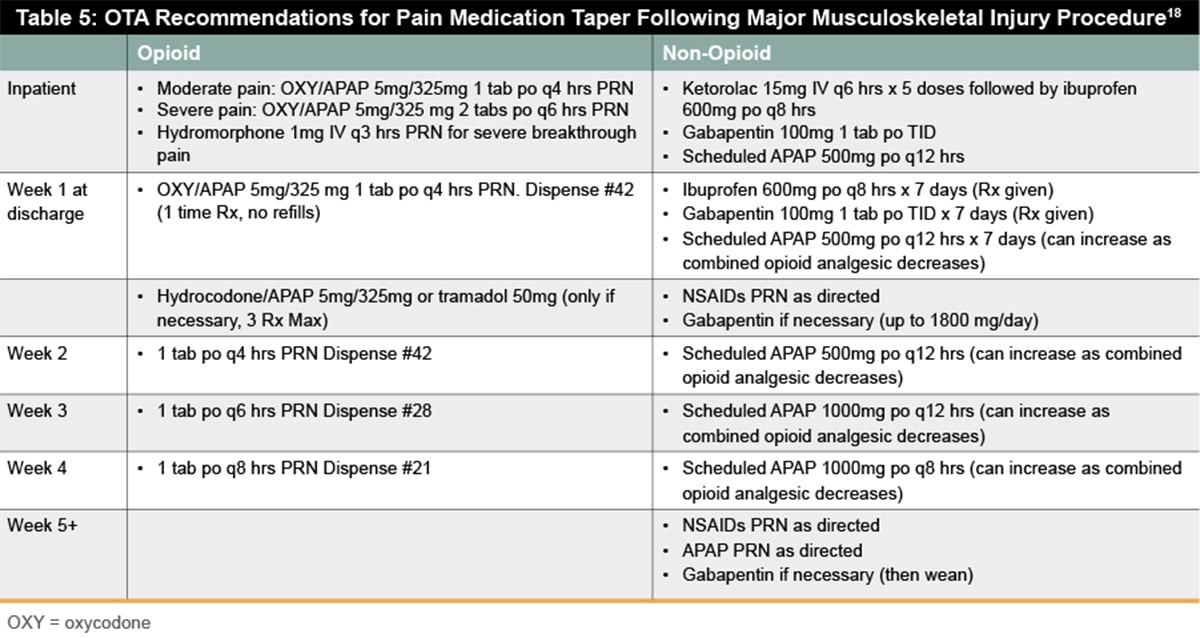
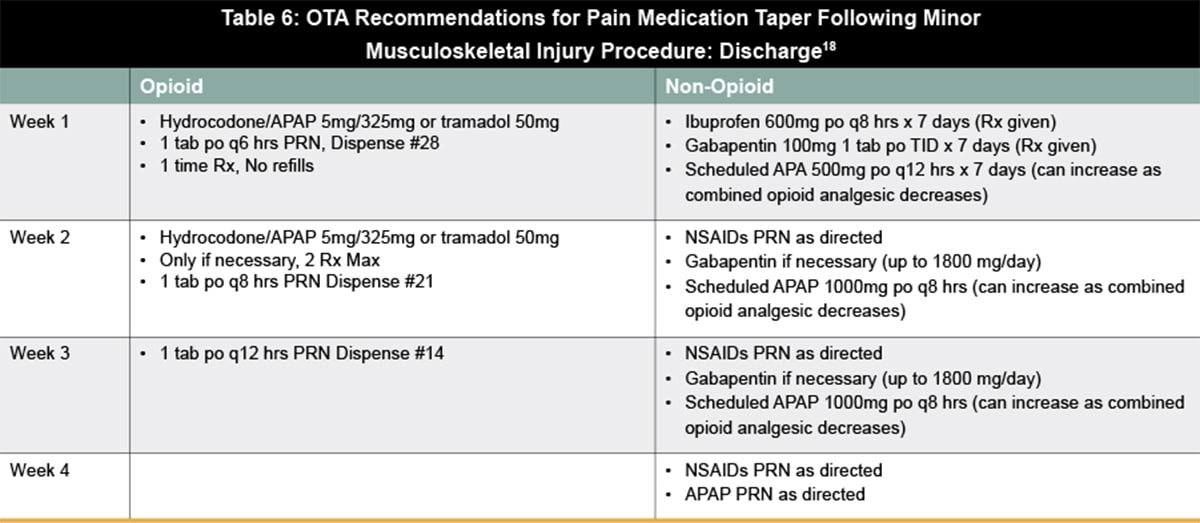
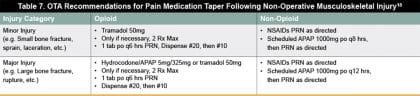
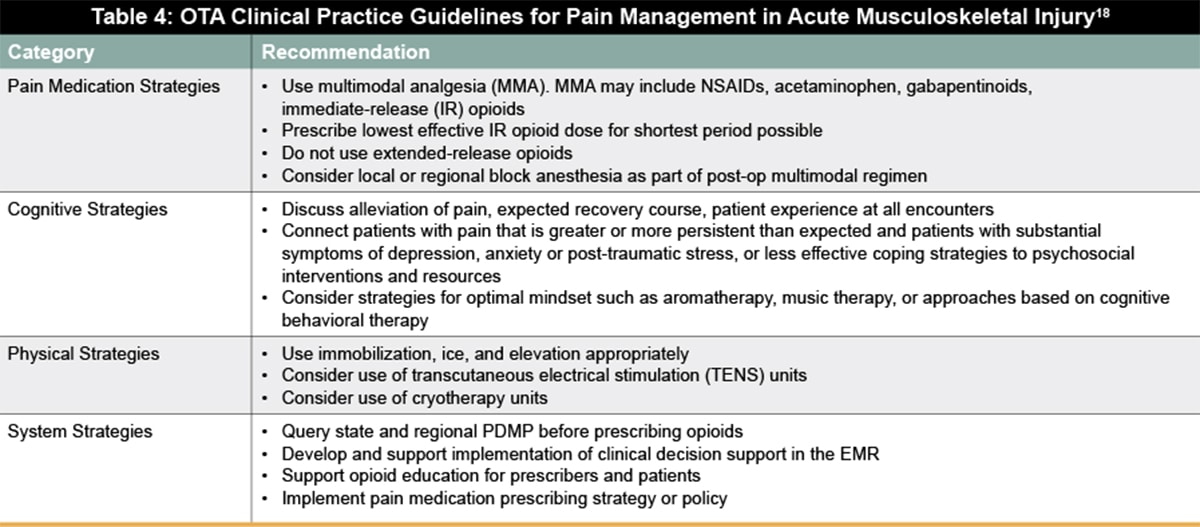 Similarly, to address the need for guidance for reducing opioid use for acute pain, the Orthopaedic Trauma Association (OTA) recently released their Clinical Practice Guidelines for Pain Management in Acute Musculoskeletal Injury. Their recommendations include pain medication strategies, cognitive strategies, physical modalities, and system tools (Table 4). The new guidelines address pain management for musculoskeletal injury based on different levels of injury sustained—major musculoskeletal injury or surgery (Table 5) , minor musculoskeletal injury or surgery (Table 6), and non-operative injuries (Table 7).18 Pain management should be discussed, and patient expectations should be managed at each visit. For opioid tolerant patients, coordination between acute pain service for inpatient management and the patient’s prescriber for outpatient management is especially important to maintain a single prescriber.18
Similarly, to address the need for guidance for reducing opioid use for acute pain, the Orthopaedic Trauma Association (OTA) recently released their Clinical Practice Guidelines for Pain Management in Acute Musculoskeletal Injury. Their recommendations include pain medication strategies, cognitive strategies, physical modalities, and system tools (Table 4). The new guidelines address pain management for musculoskeletal injury based on different levels of injury sustained—major musculoskeletal injury or surgery (Table 5) , minor musculoskeletal injury or surgery (Table 6), and non-operative injuries (Table 7).18 Pain management should be discussed, and patient expectations should be managed at each visit. For opioid tolerant patients, coordination between acute pain service for inpatient management and the patient’s prescriber for outpatient management is especially important to maintain a single prescriber.18
 Patients should receive regular follow-up to determine whether treatment goals are being met and whether opioid rotation, tapering, or discontinuation is needed.19 Opioid rotation involves changing from an existing opioid regimen to another opioid with the goal of improving therapeutic outcomes or to avoid adverse events attributed to the existing drug.20 The CDC has published a pocket guide for tapering or discontinuing opioids in patients with chronic pain to assist with implementation in clinical practice.19 It is advised to go slow (generally no more than 10% decrease per week) with the goal of maximizing pain treatment and minimizing opioid withdrawal symptoms.
Patients should receive regular follow-up to determine whether treatment goals are being met and whether opioid rotation, tapering, or discontinuation is needed.19 Opioid rotation involves changing from an existing opioid regimen to another opioid with the goal of improving therapeutic outcomes or to avoid adverse events attributed to the existing drug.20 The CDC has published a pocket guide for tapering or discontinuing opioids in patients with chronic pain to assist with implementation in clinical practice.19 It is advised to go slow (generally no more than 10% decrease per week) with the goal of maximizing pain treatment and minimizing opioid withdrawal symptoms.
 Motivational interviewing is a useful technique that can be integrated with behavioral treatment for use in a range of clinical settings, including opioid tapering and OUDs.21,22 This technique engages the patient to establish a connection, focus on a particular goal or agenda, evokes the patient’s own motivation for change, and plans a specific course of action. Motivational interviewing has been shown to improve treatment engagement and outcomes, increase medication adherence, and decrease illicit drug use. A randomized controlled study by Sullivan et al compared tapering support intervention that included motivational interviewing versus usual care. Study results showed reductions in opioid doses and pain severity ratings for both groups, and improvements in pain interference and pain self-efficacy in the motivational interviewing group.23
Motivational interviewing is a useful technique that can be integrated with behavioral treatment for use in a range of clinical settings, including opioid tapering and OUDs.21,22 This technique engages the patient to establish a connection, focus on a particular goal or agenda, evokes the patient’s own motivation for change, and plans a specific course of action. Motivational interviewing has been shown to improve treatment engagement and outcomes, increase medication adherence, and decrease illicit drug use. A randomized controlled study by Sullivan et al compared tapering support intervention that included motivational interviewing versus usual care. Study results showed reductions in opioid doses and pain severity ratings for both groups, and improvements in pain interference and pain self-efficacy in the motivational interviewing group.23
Table 8 describes guiding principles to promote optimal communication between providers and patients experiencing chronic pain.1,20 These principles can be helpful to facilitate difficult conversations with challenging patients and enable tailored pain management to maximize patient outcomes.
 In a survey by Kroll et al, pain medicine physicians reported higher rates of burnout (defined by exhaustion, cynicism, and inefficacy) compared with other specialties (61% vs 38%).25 The authors noted that occupational fatigue due to burnout puts physicians at risk for alcohol use, interpersonal difficulties, and suicidal ideation, and increases the risk for medical error. To avoid burnout, clinicians who treat patients with chronic pain should practice self-care and set healthy boundaries (eg, appropriate prescription refills, visit expectations, time limitations) with patients.4
In a survey by Kroll et al, pain medicine physicians reported higher rates of burnout (defined by exhaustion, cynicism, and inefficacy) compared with other specialties (61% vs 38%).25 The authors noted that occupational fatigue due to burnout puts physicians at risk for alcohol use, interpersonal difficulties, and suicidal ideation, and increases the risk for medical error. To avoid burnout, clinicians who treat patients with chronic pain should practice self-care and set healthy boundaries (eg, appropriate prescription refills, visit expectations, time limitations) with patients.4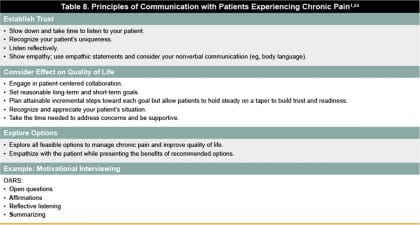
Programs that integrate behavioral health in primary care clinics (counselor, psychologist, psychiatrist, community mental health) have succeeded in expanding access, improving retention, and reducing relapse in the treatment of OUD.25 A 2017 meta-analysis conducted by Lagisetty et al analyzed 35 studies in primary care locations in eight countries.26 The authors determined that a multidisciplinary approach between primary care and specialty addiction services improves success, along with a united care team including nurses and pharmacists.
Keep on the lookout for Part 3 of this opioid education series on July 9, 2019 entitled Addressing the Opioid Epidemic: Principles of Communication and Recognizing Patient Needs for further insights on patient-centered strategies and multimodal treatment plans. Also, if you missed Part 1, Addressing the Opioid Epidemic: Reducing the Burden of Pain in a Changing Treatment Landscape, be sure to loop back for a comprehensive discussion of the state of opioids in modern practice, and an overview on the pathophysiology of pain.
To obtain credit for this activity, please click here.
References
- Florida Medical Association (FMA). Prescribing Controlled Substances: Florida Laws and Clinical Guidelines. Tallahassee, FL.
- VA South Central Mental Illness Research, Education, and Clinical Center. Pocket guide for clinicians for management of chronic pain. January 2017. Available at: https://www.mirecc.va.gov/VISN16/docs/pain-management-pocket-guide.pdf. Accessed January 26, 2019.
- Hudspeth RS. Safe Opioid Prescribing for Adults by Nurse Practitioners: Part 1. Patient History and Assessment Standards and Techniques. Journal for Nurse Practitioners. 2016;12(3):141–148
- Chang KL, Fillingim R, Hurley RW, Schmidt S. Chronic Pain Management. FP Essentials™, Edition No. 432. Leawood, KS: American Academy of Family Physicians; May 2015.
- Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain – United States, 2016. MMWR Recomm Rep. 2016;65(1):1-49.
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Sciences Policy; Committee on Pain Management and Regulatory Strategies to Address Prescription Opioid Abuse; Phillips JK, Ford MA, Bonnie RJ, eds. Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use. Washington (DC): National Academies Press (US); 2017 Jul 13. Available from: https://www.ncbi.nlm.nih.gov/books/NBK458660/doi:10.17226/2478. Accessed January 26, 2019.
- Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of Postoperative Pain: A Clinical Practice Guideline From the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131-157.
- Tater DE. Evidence for the efficacy of pain medications. Available at https://www.nsc.org/Portals/0/Documents/RxDrugOverdoseDocuments/Evidence-Efficacy-Pain-Medications.pdf. Accessed May 24, 2019.
- Gaskell H, Derry S, Moore RA, McQuay HJ. Single dose oral oxycodone and oxycodone plus paracetamol (acetaminophen) for acute postoperative pain in adults. Cochrane Database Syst Rev. 2009;(3):CD002763.
- Derry CJ, Derry S, Moore RA, McQuay HJ. Single dose oral naproxen and naproxen sodium for acute postoperative pain in adults. Cochrane Database Syst Rev. 2009;(3):CD001548.
- Derry S, Derry CJ, Moore RA. Single dose oral ibuprofen plus oxycodone for acute postoperative pain in adults. Cochrane Database Syst Rev. 2013;(6):CD010289.
- Extended-release (ER) and long-acting (LA) opioid analgesics Risk Evaluation and Mitigation Strategy (REMS). Available at: www.fda.gov/downloads/drugs/drugsafety/postmarketdrugsafetyinformationforpatientsandproviders/ucm311290.pdf. Accessed January 26, 2019.
- Department of Veterans Affairs, Department of Defense. VA/DoD Clinical Practice Guideline for Management of Opioid Therapy for Chronic Pain. 2017. Available at: https://www.healthquality.va.gov/guidelines/Pain/cot/VADoDOTCPG022717.pdf. Accessed January 26, 2019.
- Mutlu I, Abubaker AO, Laskin DM. Narcotic prescribing habits and other methods of pain control by oral and maxillofacial surgeons after impacted third molar removal. J Oral Maxillofac Surg. 2013;71(9):1500-1503.
- Lahey ET, Charest K. How many opioid pills do patients require folling third molar extraction with intravenous sedation? Journal or Oral and Maxillofacial Surgery. 2017;75(10):e361.
- Moore PA, Ziegler KM, Lipman RD, Aminoshariae A, Carrasco-Labra A, Mariotti A. Benefits and harms associated with analgesic medications used in the management of acute dental pain: An overview of systematic reviews. J Am Dent Assoc. 2018;149(4):256-265 e253.
- Abubaker AO. Oral Surgery/Dental Perspective: Evaluation and Changing Pain Protocols. Presented at: Presented at: Addressing the Opioid Epidemic: A Call to Action To Save Our Communities. Opioid HCP/Advocacy Working Group on December 3-4, 2018. 2018.
- Hsu JR, Mir H, Wally MK, Seymour RB, Orthopaedic Trauma Association Musculoskeletal Pain Task F. Clinical Practice Guidelines for Pain Management in Acute Musculoskeletal Injury. J Orthop Trauma. 2019;33(5):e152-e182.
- US Centers for Disease Control and Prevvention (CDC). Pocket guide: Tapering opioids for chronic pain. Available at: https://www.cdc.gov/drugoverdose/pdf/clinical_pocket_guide_tapering-a.pdf. Accessed January 26, 2019.
- Hooten M, Thorson D, Bianco J, et al. Pain: assessment, non-opioid treatment approaches and opioid management. August 2017. Available from: https://www.icsi.org/guidelines__more/catalog_guidelines_and_more/catalog_guidelines/catalog_neurological_guidelines/pain/. Accessed January 26, 2019.
- Rodriguez T. Motivational Interviewing for Opioid Tapering. September 5, 2017. Available at: https://www.clinicalpainadvisor.com/motivational-interviewing-for-opioid-tapering/printarticle/685068/. Accessed January 26, 2019.
- Fox AD, Masyukova M, Cunningham CO. Optimizing psychosocial support during office-based buprenorphine treatment in primary care: patients’ experiences and preferences. Subst Abus. 2016;37(1):70-5.
- Sullivan MD, Turner JA, DiLodovico C, et al. Prescription opioid taper support for outpatients with chronic pain: a randomized controlled trial. J Pain. 2017;18(3):308-318.
- US Centers for Disease Control and Prevention (CDC). Module 3: Communicating with Patients. Available at: https://www.cdc.gov/drugoverdose/training/communicating/accessible/training.html. Accessed January 26, 2019.
- Kroll H, Jesse M, Tonkin D. Do psychological workload and medical specialty predict burnout in pain medicine specialists? Journal of Pain. 2014;15(4):S39
- Lagisetty P, Klasa K, Bush C, Heisler M, Chopra V, Bohnert A. Primary care models for treating opioid use disorders: What actually works? A systematic review. PLoS One. 2017;12(10):e0186315.
