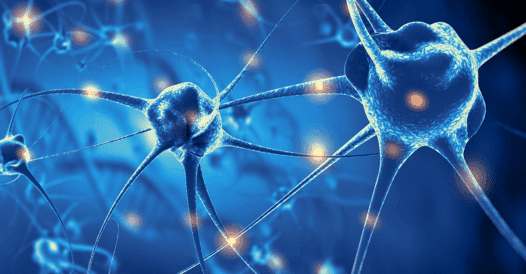
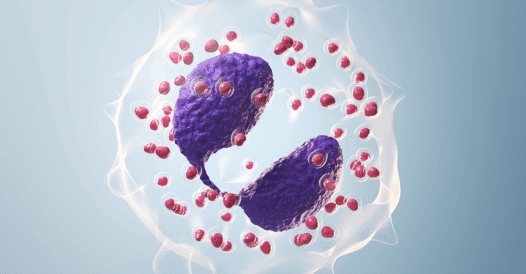
Generalized myasthenia gravis (gMG) disrupts neuromuscular transmission, creating unpredictable symptom flare-ups and placing a significant burden on patients with this rare condition. Most commonly associated with antibodies targeting the acetylcholine receptor (AChR), and less commonly with muscle specific kinase (MuSK) or low-density lipoprotein receptor–related protein 4 (LRP4), gMG has forced patients and clinicians to navigate treatments that can be difficult to tolerate, slow to act, or limited by safety concerns. The expanding availability of neonatal Fc receptor (FcRn) blockers has introduced targeted options designed to reduce pathogenic IgG and improve symptoms. Clinicians, however, lack practical, evidence-based guidance on optimizing FcRn antagonist regimens in partial responders, including interval adjustments, transitions between cyclic and consistent dosing, structured monitoring, and safe steroid tapering, which results in persistent symptoms and avoidable treatment burden. Clinicians and multidisciplinary care teams require rigorous education in optimized dosing and longitudinal management to transform the care experience for patients with gMG.
In the second activity of this CME Outfitters BriefCase series, expert faculty will differentiate MOAs, safety, and efficacy profiles of currently approved FcRn antagonists for the treatment of gMG. Faculty will incorporate strategies to identify patients with gMG who may be appropriate candidates for treatment with FcRn antagonists, and utilize an individualized approach to treatment planning for patients with gMG receiving FcRn antagonists based on the latest data as well as patient preferences.